How to Become a Sport Scientist in 6 Steps
Interested in a career in sports science but don't know where to start or even if it's a right fit for you? Read on to learn more about the profession and how Pitt can make your dream a reality!
Read More
How to Request a Strong Letter of Recommendation for Your Pitt DPT Application
Letters of recommendation play an important role in the University of Pittsburgh Doctor of Physical Therapy admissions process, providing the Admissions Committee with insight into your readiness for graduate-level education and the physical therapy profession.
Read More
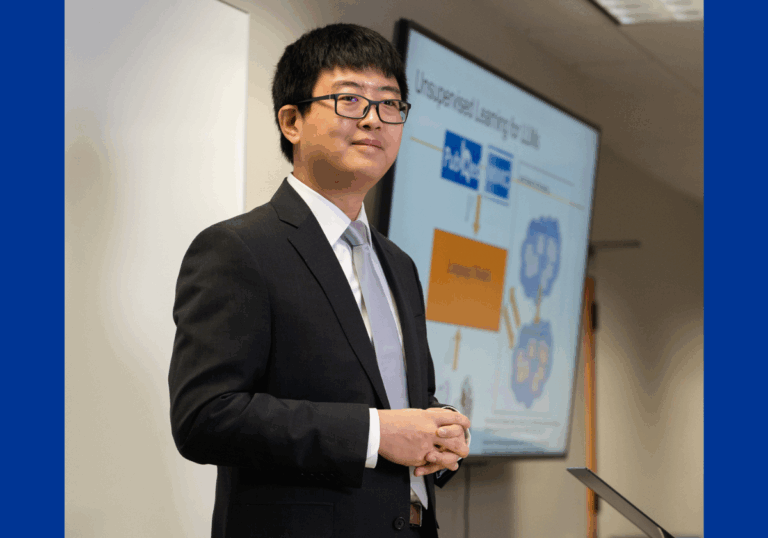
A Career Guide to your Future in Health Informatics
Health informatics (HI) applies big data to health care challenges, utilizing data analytics to drive significant advances in medical delivery and outcomes. Learn about the exciting careers in health information management!
Read More
From Dietitian Nutritionist Alumna to Faculty: Meet Assistant Professor Caroline Passerrello
Assistant Professor and Community Coordinator Caroline Passerrello attended the Dietitian Nutritionist program in 2003, then joined as a faculty member in 2013. Read on to hear about Passerrello's unique perspective as an alumna and a professor.
Read More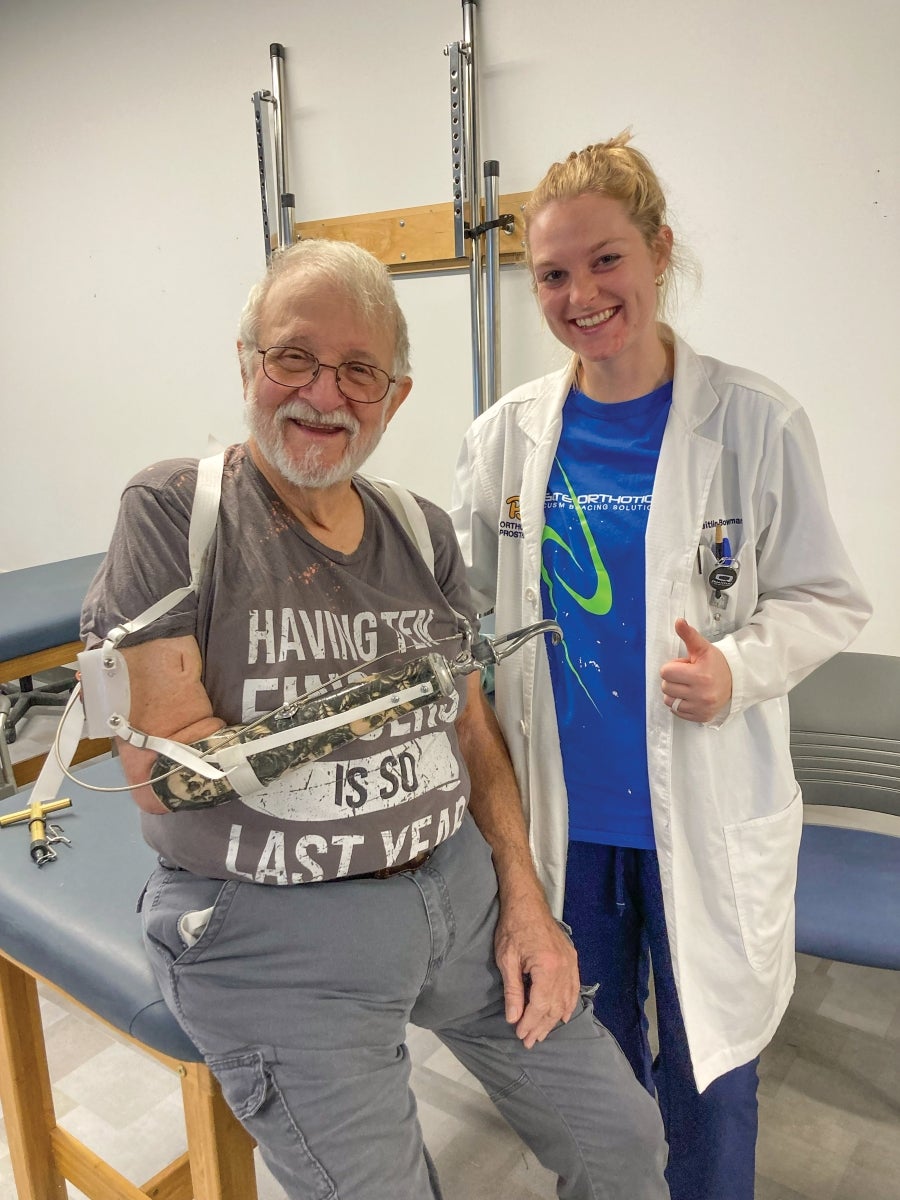
Passion for Orthotics and Prosthetics Leads to National Scholarship
Caitlin Bowman Martwinski (MSPO '24) became one of only 10 students in the country to receive a prestigious $10,000 award.
Read MoreLatest Stories
SHRS in the News
-
Physical Therapy for Knee Pain Slow to Gain Traction With CliniciansAugust 21, 2025 | MedPage Today
-
Walkers who pick up their pace get a big boost in health benefitsJuly 27, 2025 | Washington Post
-
Step inside this innovative Pitt lab that looks a lot like your grandma’s houseJuly 24, 2025 | Pittwire
-
Myth-busting vitamins: Here's what to know about some common claimsJune 16, 2025 | Pittsburgh Post-Gazette
-
Pitt's aphasia support group offers connection for those who struggle to speakJune 7, 2025 | Pittsburgh Post-Gazette